Total Hip Replacement (THR)
Overview of total hip replacement
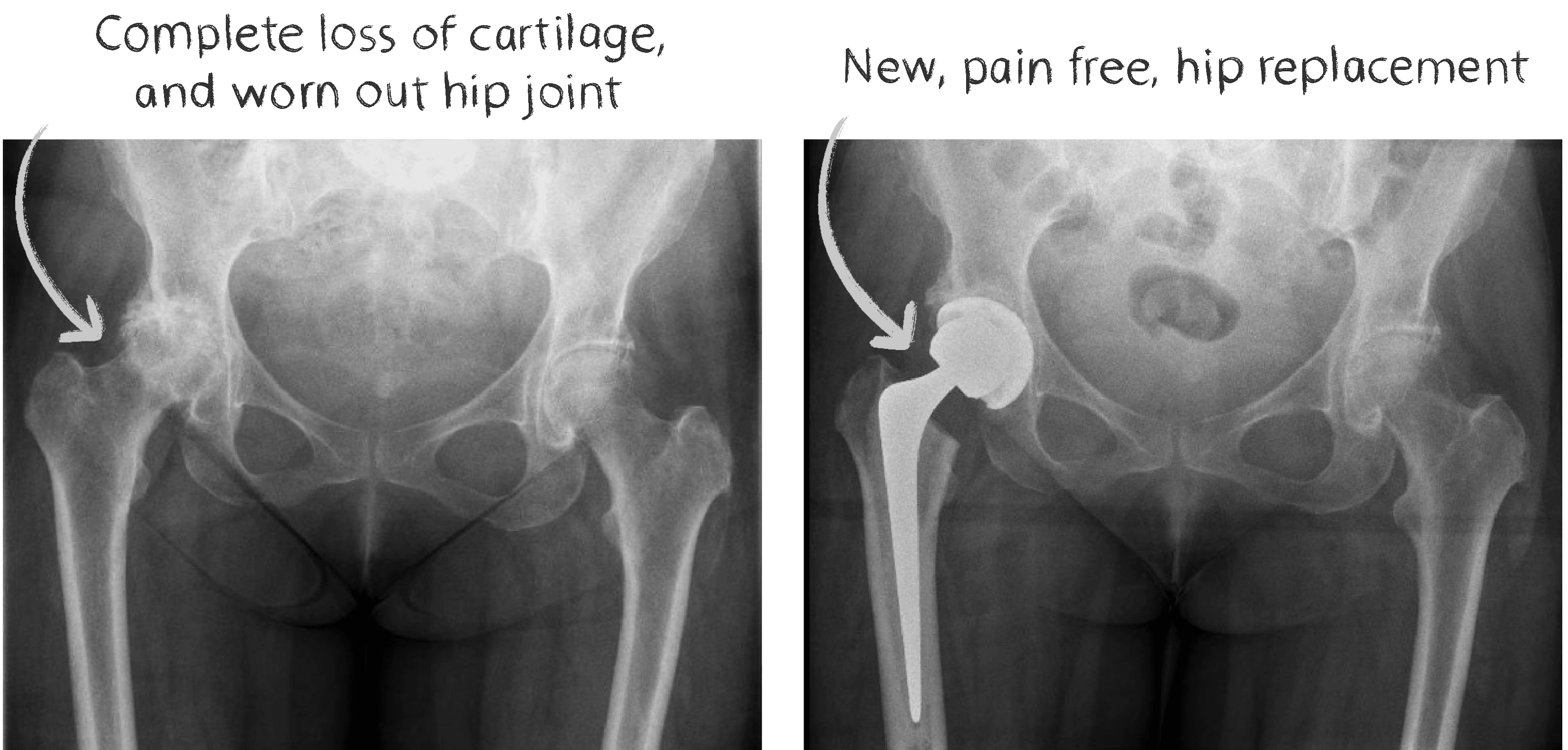
Total hip replacement is an operation where the degenerated and painful hip joint is removed and replaced with a prosthetic joint in order to treat pain and stiffness. It has been performed for nearly 60 years. It is very successful, with a success rate of over 95%. The new replacement is made up of four different components: Acetabular shell, liner, femoral head and a femoral stem.
Conditions treated with a hip replacement
Osteoarthritis is the most common reason
Inflammatory arthritis
Post-traumatic
Avascular necrosis of the femoral head
Hip dysplasia
FAQs about total hip replacement
How is the surgery performed?
We usually perform THR under spinal anaesthetic with sedation. This is when the anaesthetist injects a numbing solution into your back making you numb from the waist down. We then also give you medication via the vein to sedate you if you would like. We then position you on the operating table gently. After prepping the limb in an antiseptic agent and drapes, we remove the painful joint and replace it with a prosthetic joint. The acetabular shell with the liner is placed into the acetabulum – socket in the pelvis. The canal of the femur is exposed, and the stem is inserted down the canal. Finally, the head is placed on the femoral stem and the hip joint is connected together. The operation takes around 90-100 mins.
What approach will be used?
Hamish McLaren uses the posterior approach. This approach is by far the most common, and the “work-horse” of hip surgery. This approach provides excellent access in all individuals independent of their body shape or habitus. It produces reliable outcomes.
What should I do before my surgery?
Prehab
Undergoing active physical therapy several months prior to your surgery
This aims to strengthen your muscles, improve joint flexibility, and improve cardiovascular health to minimise complication risks and to improve function after the joint replacement
Scheduling an appointment with your GP to improve baseline health
Ensuring blood pressure is adequately treated
Medications are reviewed to ensure correct doses and timing, this is called Medication Reconciliation
If you have diabetes, make sure your blood sugars are well controlled and your HbA1c is as low as possible
Weight loss
If you are overweight, weight loss helps in many different ways
It improves access for your surgeon, leading to better component positioning
It reduces risks with anaesthetics
It has been shown to improve function and satisfaction after surgery
Can reduce the risk of infection if your BMI >40
Skin care
Your skin is the main barrier to keeping bacteria out of your joint replacement
Healthy skin is very important
Cuts and scratches may prevent the surgeon being able to perform the surgery on the day
Dry, flaking skin, cracked skin can act as a portal for bacteria to enter your body and cause both local infections and deep infections of the joint replacement
Keeping the skin moisturised, clean, and scratch-free is beneficial
Good Dentition
If you have cracked teeth or gum pain, you should consult your dentist and have a thorough dental exam.
Infection of the joint replacement can be caused by poor oral health and this is a severe complication
Stop smoking if you are a smoker
Reduce alcohol use to a minimum
What are the risks of surgery?
Infection
Dislocation
Venous thromboembolism
Periprosthetic fracture
Leg length Inequality
Nerve/vessel damage
Bleeding requiring transfusion
Non-surgical complications
- Myocardial infarction
- Strokes
- Pneumonia
Please see our page on “Risks of THA” for detailed information
When can I drive?
4 weeks post operatively
What type of Hip Implant will be used?
These days there are many different options available to surgeons. They have improved greatly over the years. There are several factors which Hamish McLaren considers when choosing the best implant for his patient. These include your age, bone quality, amount of current joint destruction, bone defects, history of osteoporosis and dislocation risks. Please refer to the section on implants for further information.
What is the recovery after surgery?
Please see our “Pre-op Handbook” for a detailed description of this.
Most people spend 1-2 days in hospital after surgery. You will begin walking on your new hip replacement the same day as surgery. Once you return home, you will require some help from friends or family. You will be using crutches for upto 4 weeks. You will return to our clinics around 10-14 days after the operation for the wound to be inspected and then again 6 weeks after surgery for your final review. Please see our “Pre-Op hand book” for a detailed description of your journey through a total hip or knee replacement.
What activities can I do / not do after surgery?
You will slowly be able to increase your level of activity as the weeks progress. Generally speaking, you can begin walking on the hip immediately. You can start going out of the house for short walks once home and the distance can slowly increase as your symptoms improve. By 6 weeks most people are re-starting exercise and by 3 months, most are back to their usual activities. Studies show by 6 months most of the patients have fully recovered. Dislocation risk is highest during the first 3 months postoperatively. We do not want you bending the hip excessively or rotating/twisting your body around the hip during this period.
When can I return to work?
This is highly dependent upon your occupation
Sedentary office-based work - 6 weeks or potentially earlier
Heavier labour-type jobs - can be up to 3 months



