A Deeper Dive in to Robotic Assisted TKA
Robots have been used in orthopaedic surgery for over 20 years. Over this time, they have evolved tremendously. The most common use for robots in the orthopaedic field is total joint arthroplasty (TJA), and in particular for the hip and knee.
There are three main components to robotic joint replacement
Navigation to allow the robot to “see”
The Robotic arm to which a cutting saw or burr can be attached
Software to allow the surgeon to plan the operation and make changes during the case
Current methods and limitations of traditional TKA
The current situation is most surgeons use rods placed either inside the canal of the main bones or on the outside to get a rough idea of the alignment. They then attached cutting jigs that guide the saw blade while cutting. This system allows for the possibility of sizable bone cut errors. The rods don’t always show the true alignment, the saw can skive in the jigs, the pins holding the jigs can wobble. However, it is still the most common way of performing TKA and despite these issues, over 80% of the patients are very satisfied with their TKA.
Navigation technology:
A step forward
The next advancement in improving TKA outcomes was navigation. This technology uses steel pins placed in the femur and tibia, with reflective balls attached that a camera tracks. The surgeon then marks the joint surfaces with a stylus, allowing the system to display the knee's alignment for more precise planning. However, issues like jig misplacement or saw errors can still occur, meaning inaccuracies are still possible even with this system. Despite knowing the desired alignment, conventional tools leave room for user error, making it difficult to achieve perfect results every time.
Robotics improves on these issues and brings accuracy and precision.

The patient undergoes a low dose CT scan of the affected limb several weeks before the operation

The images are uploaded onto the Robotic software allowing it to know the exact 3D structure of the joint and the alignment of the entire limb

The surgeon can now plan the operation, chose the size of the components needed, plan the initial positioning of the components

At the start of the operation pins are placed and reflective markers attached which allows the robot to “see” the limb

A stylus is used to mark out the bone surfaces and joint surfaces which allows the robot to now “see” the joint. The robot ensures the joint looks exactly the same as the 3D model, so there are no errors

The knee is taken through a range of motion and stressed

The surgeon then uses this information to personalise the exact balance and position of the prosthesis
The robotic arm and saw are brought in and the cuts are made exceptionally accurately – to within 0.3-0.5mm
Once the cuts have been completed, trial components are used and the knee is checked for alignment and balance.

Once the surgeon is happy with the alignment and balance, the definitive prostheses are installed and the knee is closed
There are several different robots currently being used for TKA. They are all very good at helping the surgeon perform TKA.
Advantages of Image-Based Robots over Imageless Robots
CT based image guidance
This allows a robot to be much more accurate than imageless robotic TKA
It also removes any error that can come from inaccurate referencing of the joint surfaces with the stylus, as the imaged -based robot ensures it matches the 3D image from the CT scan.
The surgeon can identify old metalwork in the bone from previous operations and determine if it will interfere with the joint replacement or not, prior to the operation starting.
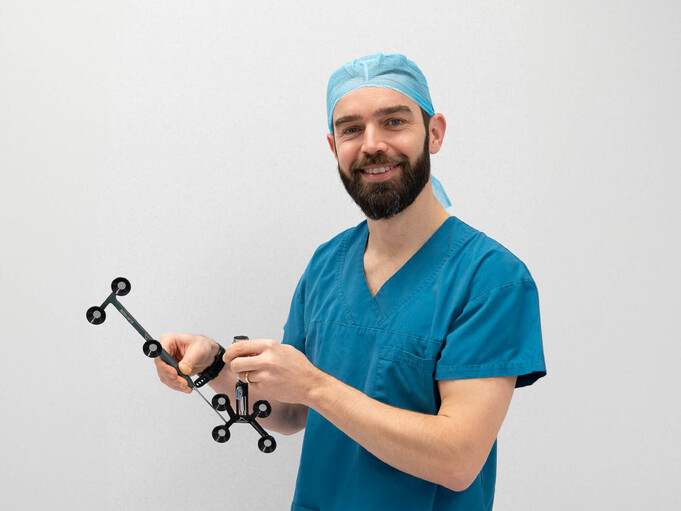
Haptic Boundary
The robot Mr. McLaren uses is the only robotic arm that has haptic feedback. It knows the exact location of the bone margins. It will not allow the surgeon to cut outside this boundary. This reduces trauma to surrounding soft tissues and reduces the risk of damage to nerves and vessels. This in turn reduces post operative pain and faster recovery.
The robot Mr. McLaren uses can also robotically assist with
Total hip replacement and unicompartmental knee replacement which other robots currently cannot.