Joint Replacement FAQs
Deciding to undergo a total hip or knee replacement is one of the biggest decisions you will make.
There are many questions orthopaedic surgeons are asked by our patients about total hip and knee replacements. Here are some of the common questions:
How long will my joint replacement last?
How good will my joint replacement be?
Will I be able to run on my joint replacement?
What are the common things that go wrong with joint replacements?
What are the catastrophic problems that could occur with joint replacements?
What can I do to improve my chances of a good outcome after joint replacement surgery?
How long will my joint replacement last?
While there is no easy answer to this question, 90% of total hip replacements performed in NZ remain inside the patient for at least 15 years without revision*. Various factors influence this longevity, including age, gender, BMI, and the precision of the surgery itself.
*This information is from the NZ Joint Registry, where we keep information on nearly all of our patients undergoing joint replacement
Assuming your joint replacement is successful and initially provides complete pain relief and excellent range of motion, several issues can arise over time that may require revision. These include aseptic loosening, where the mechanical fixation of the joint loosens, septic loosening which occurs if an infection develops, fractures of the bone around the joint due to trauma, and repeated dislocations, leading to instability.
In recent years, infection has become a more common reason for revising joint replacements. This is particularly true as more people are requesting joint replacements at a younger age. The longer a joint replacement is implanted, the more time it is exposed to potential infection risks. Infections can occur at any time after surgery, even years post-implantation. If an infection arises after this period, it is often due to a "seeding" event through the bloodstream.
Certain health conditions also contribute to an increased risk of infection and early revision of joint replacements. These conditions include morbid obesity (BMI over 40), diabetes, inflammatory or autoimmune disease and smoking, all of which elevate the chances of complications following surgery.
The age at which you choose to have your joint replacement plays a significant role in determining the longevity of the implant. Older individuals are more likely to live out their lives with the original joint replacement, as they typically exert less force on the joint. In contrast, younger individuals tend to use the joint more actively, subjecting it to greater stress, which can increase the likelihood of requiring a revision.
Fractures of the bones around a joint replacement are also becoming more frequent in New Zealand, driven by two main factors. Firstly, more people are undergoing joint replacements and our patients with joint replacements are living longer. As we age, our bone density and strength declines making us susceptible periprosthetic fractures. In some cases, when a bone fractures around a joint replacement, surgeons may need to revise part of the joint or, in more severe cases, the entire joint.
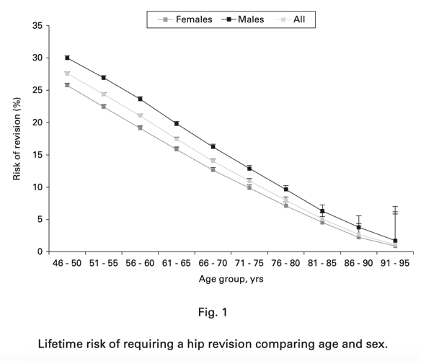
Nugent M, Young SW, Frampton CM, Hooper GJ. The lifetime risk of revision following total hip arthroplasty. Bone Joint J. 2021;103-B(3):479-485. doi:10.1302/0301-620X.103B3.BJJ-2020-0562.R2
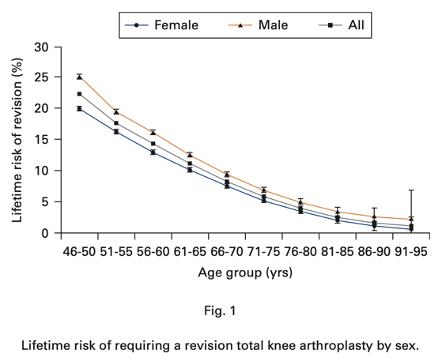
Stone B, Nugent M, Young SW, Frampton C, Hooper GJ. The lifetime risk of revision following total knee arthroplasty. Bone Joint J. 2022;104-B(2):235-241. doi:10.1302/0301-620X.104B2.BJJ-2021-0890.R1
How good will my joint replacement be?
This too is a very hard question to answer. On average 90-95% of patients are satisfied with their total hip replacement and 80-85% of patients are satisfied with their total knee replacement.
Orthopaedic surgeons have extensively studied patient satisfaction following joint replacement surgery, but we still encounter challenges in accurately measuring and defining satisfaction.
There are many variables that contribute to one patient feeling satisfied and another feeling unsatisfied. Preoperative expectations play a significant role. What the patient expects regarding their new joint can heavily influence their level of satisfaction.
Preoperative pain and function are also critical. Patients who experience significant pain or limited mobility before surgery may have different outcomes compared to those with less severe symptoms. The degree of arthritis present prior to surgery can further impact results.
A patient's overall health before surgery is another important factor. Those with better preoperative health often recover more smoothly. Additionally, if the patient has other painful joints, this can continue to cause discomfort, even after the joint replacement.
Finally, satisfaction can be affected if a patient develops complications post-operatively, which can hinder recovery and overall satisfaction with the procedure.
Will I be able to run on my hip or knee joint replacement?
Most orthopaedic surgeons would advise that joint replacements are not designed to withstand the impact of running. The forces exerted on the hip joint during various activities have been studied and measured as follows:
Walking: approximately 2.5 times your body weight (250%)
Jogging: approximately 5.2 times your body weight (520%)
Stumbling: approximately 8.7 times your body weight (870%)
These forces can also be generalised to knee replacements.
Interestingly, many hip replacement patients continue to engage in activities such as hiking, skiing, surfing, and cycling. For instance, when skiing, the forces across the hip joint range from 4.1 to 7.8 times body weight.
The more force applied to the prosthesis, and the more frequent these forces are applied, the more wear is likely to occur on the bearing surface. This could lead to loosening of the prosthesis or wear on the bearing surface, both of which may require surgical intervention.
Instead of asking, "Will I be able to run on my hip replacement?" it might be more appropriate to ask, "Will I return to running on my joint replacement?" The article cited below offers a valuable insight into running after total hip and total knee replacements.
Antonelli B, Teng R, Breslow RG, Jamison M, Hepinstall M, Schwarzkopf R, Moschetti WE, Chen AF. Few Runners Return to Running after Total Joint Arthroplasty, While Others Initiate Running. J Am Acad Orthop Surg Glob Res Rev. 2023 Apr 19;7(4):e23.00019. doi: 10.5435/JAAOSGlobal-D-23-00019. PMCID: PMC10118379.
What are the common things that go wrong with total hip replacements?
Thankfully, most hip replacements go smoothly, and patients are generally satisfied with the outcomes.
Limping can occur after surgery, usually due to significant abductor muscle weakness that existed preoperatively. The gluteus medius and minimus muscles often atrophy when we experience severe osteoarthritis (OA) in the hip, leading to reduced walking ability. Even after the hip replacement, it can take up to 18 months to fully rebuild these muscles.
Bruising and swelling are common post-surgery. Visible bruising occurs when bleeding comes close to the surface of the skin, often following the forces of gravity, causing it to move down the leg. Swelling can vary significantly from patient to patient and may affect the whole limb, down to the ankle. In some cases, swelling may take up to three months to settle.
Scar tenderness or sensitivity is another post-operative issue. Although the wound around hip replacements tends to heal quickly, some patients may develop a tender or sensitive scar. This discomfort typically resolves within six weeks to three months, and simple massage and scar stretching can help alleviate the sensitivity.
What are the catastrophic complications that can occur with joint replacement?
For a complete list of potential complications from total hip and knee replacements, please refer to the complications page.
Death
Though rare, the risk in NZ is 0.18% based on data from 2007-2011 (Hider et. al. NZMJ April, 2016, Vol 129, No. 1432).
Damage to major nerves or arteries
In hip replacement, there is a risk of damage to the sciatic nerve or injury to the femoral artery.
In knee replacement, the tibial nerve or vessels can be affected.
Major medical complications
These can include severe conditions such as:
Myocardial infarction (heart attack)
Stroke
Severe Pulmonary Embolus (blood clot in the lungs)
What are the common things that go wrong with total knee replacements?
Thankfully, most knee replacements proceed smoothly, leaving patients satisfied with the results.
Numbness over the outer side of the knee is a common post-surgery complaint. Due to the way the cutaneous skin nerves travel, the skin on the outer (lateral) side of the wound often loses sensation. While this typically improves over the years, it may never fully return to normal.
Inability to squat or kneel perfectly is another common issue. The range of motion before surgery is the biggest predictor of post-operative flexibility. Arthritic knees are often stiff before the operation, and after total knee replacement, the joint usually can't bend enough for deep squats. Additionally, some people find kneeling difficult after TKA due to scar sensitivity and stiffness.
A mechanical feeling is often reported with total knee replacements. Unlike hip replacements, which can feel so natural that patients may forget they've had surgery, knee replacements often retain a more noticeable mechanical sensation.
Will my joint replacement set off the sensors at the airports?
Yes. They are made of a large amount of either titanium, stainless steel or Coblat-Chrome alloy. Don’t worry, the security staff at airports are very familiar with patients and joint replacements. They will usually double check with their “wand”. You no longer need written evidence such as “Joint Replacement Cards”.
What happens if the Robot Assistance stops working during the operation?
Although this is very uncommon, if the robot assistance does stop working, we can usually restart it without issue. In the rare event that the robot cannot be restarted, I can seamlessly continue the procedure using standard instrumentation, ensuring the surgery proceeds safely and effectively.
What can I do to improve my chances of a good outcome after total hip replacement?
There is an excellent video published on YouTube by Dr. Mike Evans about preparing for your joint replacement. I strongly recommend you watch it. The link is below. In case the link changes – the title is “Hip and Knee Replacement Doc Mike Evans”.
Prehab
Engaging in active physical therapy several months before surgery is crucial. This helps strengthen muscles, improve joint flexibility, and boost cardiovascular health, all of which minimise complications and improve post-surgery function.
Visit Your GP
Schedule an appointment with your GP to ensure your baseline health is optimised:
Ensure your blood pressure is well-managed.
Review medications for correct doses and timing, a process known as Medication Reconciliation.
If you have diabetes, keep your blood sugars controlled and aim for a low HbA1c level.
Weight Loss
If you're overweight, losing weight before surgery offers several benefits:
It allows for better surgical access and improves component positioning.
Reduces anaesthetic risks.
Improves overall function and satisfaction after surgery.
Lowers the risk of infection, especially if your BMI is over 40.
Skin Care
Healthy skin is essential to preventing infection. Cuts, scratches, or dry, cracked skin can introduce bacteria that might lead to infections. Keep your skin moisturised, clean, and free from any injuries in the lead-up to surgery.
Stop smoking and limit alcohol
If you smoke, stopping will greatly benefit your recovery. Reducing alcohol intake to a minimum is also recommended to lower surgical risks and improve recovery outcomes.


